Pharmacy Benefit Management Market Size Report, Industry Share, Analysis, 2032

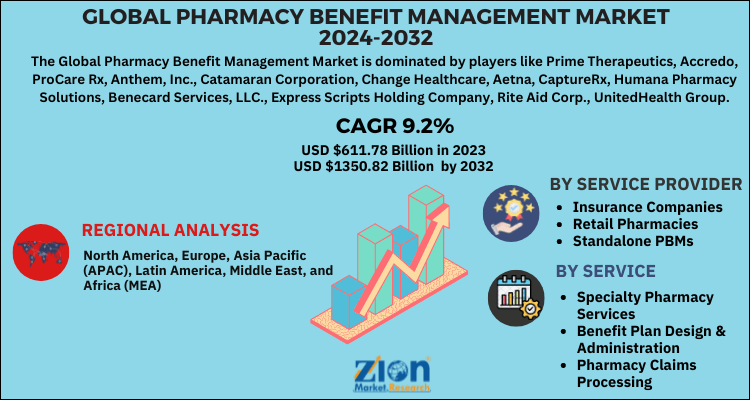
Pharmacy Benefit Management Market By Service (Specialty Pharmacy Services, Benefit Plan Design & Administration, Pharmacy Claims Processing, Formulary Management, and Others), By Service Provider (Insurance Companies, Retail Pharmacies, and Standalone PBMs), and By Region: Global Industry Analysis, Size, Share, Growth, Trends, and Forecast, 2024-2032
| Market Size in 2023 | Market Forecast in 2032 | CAGR (in %) | Base Year |
|---|---|---|---|
| USD 611.78 Billion | USD 1350.82 Billion | 9.2% | 2023 |
Description
Global Pharmacy Benefit Management Market: Industry Analysis
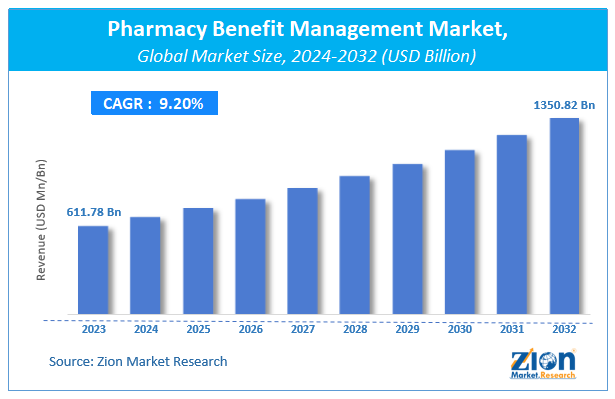
The global Pharmacy Benefit Management Market size was valued at USD 611.78 Billion in 2023 and is predicted to reach USD 1350.82 Billion by the end of 2032. The market is expected to grow with a CAGR of 9.2% during the forecast period. The report analyzes the global Pharmacy Benefit Management Market's growth drivers, restraints, and impact on demand during the forecast period. It will also help navigate and explore the arising opportunities in the Pharmacy Benefit Management industry.
Key Insights
- As per the analysis shared by our research analyst, the pharmacy benefit management market is anticipated to grow at a CAGR of 9.2% during the forecast period (2024-2032).
- The global pharmacy benefit management market was estimated to be worth approximately USD 611.78 billion in 2023 and is projected to reach a value of USD 1350.82 billion by 2032.
- The growth of the pharmacy benefit management market is being driven by rising consumer spending on prescription drugs is soaring the demand for pharmacy benefit management.
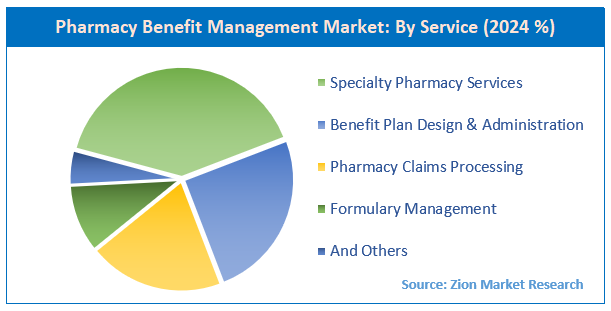
- Based on the service, the specialty pharmacy services segment is growing at a high rate and is projected to dominate the market.
- On the basis of service provider, the insurance companies segment is projected to swipe the largest market share.
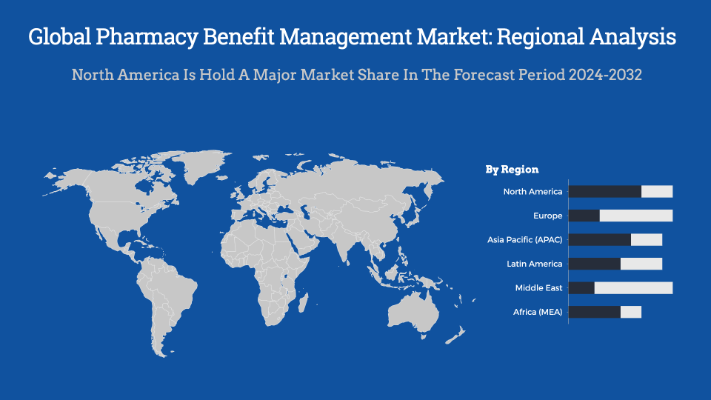
- By region, North America is expected to dominate the global market during the forecast period.
Global Pharmacy Benefit Management Market: Overview
The pharmacy benefit manager acts as a third-party administrator. Pharmacy benefit management is an administration of prescription drug programs that monitors, administers, and handles all the issues concerned with healthcare and facilitates drug benefit programs for the organization’s employers. It aids in providing the medical services and prescribed medicines at low costs to the employers.
The cost reduction is done with the help of rebates from various drug manufacturers, undergoing contracts with various pharmacies, processing & compensating the prescribed drug claims, and working with government programs & self-insured companies.
The pharmacy benefit management (PBM) calls out the lists of the prescription drugs which enclose all the drugs covered in the plans where the manufacturers are liable to offer discounts. The pharmacy benefit management can be varied from flexible and diverse programs ranging from the big to small in size. Some of the applications of the pharmacy benefit manager include medication therapy programs, assessing the clinical programs for the huge populations, less expensive therapeutic alternatives, awareness regarding tablet splitting, and mail order service.
Global Pharmacy Benefit Management Market: Growth Factors
One of the factors that are driving the global pharmacy benefit management market is the urgent need to eliminate or reduce medication errors. It is raising healthcare expenditure costs across the globe. Also, the rising consumer spending on prescription drugs is soaring the demand for pharmacy benefit management. The PBM helps in managing and planning the formulary concerning the customer wants, negotiating discounts, different rebates from drug manufacturers, processing the claims concerned with the prescription, and contracting with different pharmacies.
To improve the customer value and reduce the cost of prescription drugs, different tools are adopted by the PBMs like pharmacy discount cards, drug utilization review, disease management, manufacturer’s discount, e-prescribing, drug formulary, mail-service pharmacies, pharmacy networks, and many more.
Recent Development
- In June 2025, Capital Rx, a transparent PBM, acquired Amino Health to integrate medical and pharmacy claims data on one platform, enhancing transparency and member experience in health benefits.
- In November 2023, OptumRx, the PBM of UnitedHealth, announced it would add eight popular insulin products to preferred status on its standard formulary for U.S. commercially insured members.
- In Feb 2023, CVS Health acquired Oak Street Health for $10.6 billion, expanding its vertical integration strategy by adding senior-focused primary care centers to complement its PBM, retail pharmacy, and insurance businesses.
Global Pharmacy Benefit Management Market: Report Scope
| Report Attributes | Report Details |
|---|---|
| Report Name | Pharmacy Benefit Management Market |
| Market Size in 2023 | USD 611.78 Billion |
| Market Forecast in 2032 | USD 1350.82 Billion |
| Growth Rate | CAGR of 9.2% |
| Number of Pages | 207 |
| Key Companies Covered | Prime Therapeutics, Accredo, ProCare Rx, Anthem, Inc., Catamaran Corporation, Change Healthcare, Aetna, CaptureRx, Humana Pharmacy Solutions, Benecard Services, LLC., Express Scripts Holding Company, Rite Aid Corp., UnitedHealth Group, SS&C Technologies, Inc., and CVS Health |
| Segments Covered | By service, By business model, By end-user and By Region |
| Regions Covered | North America, Europe, Asia Pacific (APAC), Latin America, Middle East, and Africa (MEA) |
| Base Year | 2023 |
| Historical Year | 2018 to 2022 |
| Forecast Year | 2024 - 2032 |
| Customization Scope | Avail customized purchase options to meet your exact research needs. Request For Customization |
Global Pharmacy Benefit Management Market: Segmentation
The global pharmacy benefit management market can be segmented into service, business model, end-user, and region. All the segments have been analyzed based on present and future trends and the market is estimated from 2024 to 2032.
By Service, the market can be segmented into mail order service, benefit plan design & consultation, drug formulary management, specialty pharmacy services, and others. The specialty pharmacy services segment holds hegemony over others as the market consolidates with growing acquisitions and mergers.
By Business Model, the market can be segmented into health insurance management, employer-sponsored programs, and government health programs.
By End-User, the market can be segmented into outpatient pharmacies, inpatient pharmacies, retail pharmacies, mail-order pharmacies, pharmacy benefit management organizations, and others. The inpatient pharmacies can further be segmented into long term care facilities and acute care settings. The outpatient pharmacies can be segmented into hospital retail settings and outpatient clinics.
The Retail Pharmacy segment holds the largest share in the global pharmacy benefit management market as these services help patients to avail drugs at an affordable price.
The Regional segment includes the current and forecast demand for North America, Europe, Asia Pacific, Latin America, and the Middle East and Africa.
Pharmacy Benefit Management Market Dynamics
Key Growth Drivers
The Pharmacy Benefit Management (PBM) market is primarily driven by the escalating cost of prescription drugs, which compels health plan sponsors, including employers and health insurers, to seek effective solutions for cost containment. PBMs leverage their massive purchasing power to negotiate rebates and discounts with pharmaceutical manufacturers and pharmacies, ultimately aiming to lower drug costs for their clients. The rising prevalence of chronic diseases globally is another major driver, as this trend leads to a greater volume and complexity of prescriptions, increasing the need for sophisticated medication management services. Furthermore, the shift toward value-based care models, which focus on patient outcomes rather than the volume of drugs dispensed, is fueling demand for PBMs to help ensure patients receive the most effective and cost-efficient treatments.
Restraints
The PBM market faces significant restraints, primarily stemming from a pervasive lack of transparency in business practices. PBMs have been widely criticized for their complex pricing models, such as "spread pricing," where they charge health plans more for a drug than they reimburse the pharmacy, and "rebate retention," where they keep a portion of the rebates negotiated with drug manufacturers. This opacity has led to increased scrutiny from regulators, lawmakers, and consumer advocacy groups, who argue that these practices drive up drug costs and reduce savings for patients and payers. The ongoing push for regulatory reform and litigation against PBMs in various states poses a significant threat to their current business models. Furthermore, the high concentration of the market, with a few large PBMs controlling a vast majority of the market share, limits competition and reduces negotiating power for smaller pharmacies and health plans.
Opportunities
The PBM market is presented with significant opportunities for innovation and growth. The increasing adoption of digital health technologies, such as Artificial Intelligence (AI) and machine learning, is enabling PBMs to develop more sophisticated tools for data analytics, fraud detection, and personalized medication management. This allows for more precise formulary design and can improve patient adherence to treatment plans. Another key opportunity lies in the burgeoning market for specialty drugs, which are high-cost, high-touch medications for complex and rare diseases. PBMs with robust specialty pharmacy services are well-positioned to manage the intricate logistics and patient support required for these drugs. The expansion of government-sponsored health programs and a growing emphasis on medication therapy management (MTM) services also offer new avenues for PBMs to expand their role beyond traditional claims processing.
Challenges
The PBM market faces several critical challenges. The most pressing is the intense regulatory and political scrutiny it is under, with many in Congress and state legislatures exploring ways to increase transparency and rein in PBM practices. This regulatory uncertainty creates a challenging environment for business planning and long-term investment. Another major challenge is the pushback from independent and community pharmacies, who argue that PBM practices, such as "direct and indirect remuneration" (DIR) fees and low reimbursement rates, are squeezing their profit margins and threatening their viability. This can lead to network disruptions and reduced access to care for patients. Furthermore, as vertical integration continues with large PBMs merging with health insurers and retail pharmacies, a potential conflict of interest arises, leading to concerns that PBMs will favor their own affiliated services over more cost-effective options from competitors.
Global Pharmacy Benefit Management Market: Regional analysis
North America holds the largest share in the global pharmacy benefit management market owing to the significant surge in the number of Medicare prescription drug program subscribers. The pharmacy benefits merger also helps in checking on whether a generic or branded drug will be fit for the patient. Moreover, there is significant growth in the region due to the proliferation of the pharmaceutical and biopharmaceutical sector. The region has a huge base of pharmacy benefit management vendors.
Europe is a growing region in the global pharmacy benefit management market due to the added benefits of the PBM. The region has a good profit margin from generic drugs.
Asia Pacific is anticipated to witness huge growth during the forecast period due to the constant technological advancements in developing countries like India and China.
Global Pharmacy Benefit Management Market: Competitive Players
Some of the significant players in the global pharmacy benefit management market are:
- Prime Therapeutics
- Accredo
- ProCare Rx
- Anthem, Inc.
- Catamaran Corporation
- Change Healthcare
- Aetna
- CaptureRx
- Humana Pharmacy Solutions
- Benecard Services, LLC.
- Express Scripts Holding Company
- Rite Aid Corp.
- UnitedHealth Group
- SS&C Technologies, Inc.
- And CVS Health.
Global Pharmacy Benefit Management Market: Segmentation
By Service
- Specialty Pharmacy Services
- Benefit Plan Design & Administration
- Pharmacy Claims Processing
- Formulary Management
- And Others
By Service Provider
- Insurance Companies
- Retail Pharmacies
- Standalone PBMs
Global Pharmacy Benefit Management Market: Regional Segment Analysis
- North America
- The U.S.
- Canada
- Europe
- France
- The UK
- Spain
- Germany
- Italy
- Rest of Europe
- Asia Pacific
- China
- Japan
- India
- South Korea
- Southeast Asia
- Rest of Asia Pacific
- Latin America
- Brazil
- Mexico
- Rest of Latin America
- Middle East & Africa
- GCC
- South Africa
- Rest of Middle East & Africa
What Reports Provides
- Full in-depth analysis of the parent market
- Important changes in market dynamics
- Segmentation details of the market
- Former, on-going, and projected market analysis in terms of volume and value
- Assessment of niche industry developments
- Market share analysis
- Key strategies of major players
- Emerging segments and regional markets
- Testimonials to companies in order to fortify their foothold in the market
Table Of Content
FrequentlyAsked Questions
The pharmacy benefit manager acts as a third-party administrator. Pharmacy benefit management is an administration of prescription drug programs that monitors, administers, and handles all the issues concerned with healthcare and facilitates drug benefit programs for the organization’s employers. It aids in providing the medical services and prescribed medicines at low costs to the employers.
The Pharmacy Benefit Management Market was valued at USD 611.78 Billion in 2023.
The Pharmacy Benefit Management Market is expected to reach USD 1350.82 Billion by 2032, growing at a CAGR of of 9.2% between 2024 to 2032.
One of the factors that are driving the global pharmacy benefit management market is the urgent need to eliminate or reduce medication errors. It is raising healthcare expenditure costs across the globe. Also, the rising consumer spending on prescription drugs is soaring the demand for pharmacy benefit management. The PBM helps in managing and planning the formulary concerning the customer wants, negotiating discounts, different rebates from drug manufacturers, processing the claims concerned with the prescription, and contracting with different pharmacies.
Pharmacy Benefit Management Market players such as Prime Therapeutics, Accredo, ProCare Rx, Anthem, Inc., Catamaran Corporation, Change Healthcare, Aetna, CaptureRx, Humana Pharmacy Solutions, Benecard Services, LLC., Express Scripts Holding Company, Rite Aid Corp., UnitedHealth Group, SS&C Technologies, Inc., and CVS Health.
The Regional segment includes the current and forecast demand for North America, Europe, Asia Pacific, Latin America, and the Middle East and Africa.
HappyClients
Zion Market Research
Tel: +1 (302) 444-0166
USA/Canada Toll Free No.+1 (855) 465-4651
3rd Floor,
Mrunal Paradise, Opp Maharaja Hotel,
Pimple Gurav, Pune 411061,
Maharashtra, India
Phone No +91 7768 006 007, +91 7768 006 008
US OFFICE NO +1 (302) 444-0166
US/CAN TOLL FREE +1 (855) 465-4651
Email: sales@zionmarketresearch.com
We have secured system to process your transaction.
Our support available to help you 24 hours a day, five days a week.
Monday - Friday: 9AM - 6PM
Saturday - Sunday: Closed